
An Intensive Care Unit (ICU) is a department in the hospital that provides specialized care for patients. It is sometimes also called a critical care unit. The health care team in the ICU has experience treating patients with severe and life-threatening illnesses or injuries.
While your family member is in the ICU, they will be checked often by the health team, and may have many machines attached to them. Some of these machines are used to monitor the patient’s conditions – for example, to check heart rate. Other machines provide medications, or support failing organs, such as breathing machines that help the person breathe.
There are lots of things happening in the ICU. Dr. Heyland explains how My ICU Guide can help you understand what’s going on.
*Click CC in the play bar or C on your keyboard for subtitles/closed captions
ICU Terms and Treatments
By learning more about medical terms and treatments, and legal requirements, you can make better support your family member in the ICU.
ICU Medical and Legal Terms
Here are some common medical and legal terms that are important to know
Advanced Care Planning (ACP)
Allow natural death
Comfort Measures
End-of-life care
Family Meeting
Frailty
Hospice Care
Hospice care strives to help patients and families by addressing physical, psychological, social, spiritual and practical issues along with their associated expectations, needs, hopes and fears. It can help prepare for and manage self-determined life closure and the dying process and help patients and families cope with loss and grief during the illness and bereavement.
Goals of Care
Organ Donation
Transplantation is necessary because the recipient’s organ has failed or has been damaged by disease or injury. Make sure your family knows if you wish to be an organ and tissue donor. Even if you have registered as a donor, health professionals may still need to ask your family for consent before recovering organs or tissue. Donation can take place only if your family consents at the time of death.
Rounds
Palliative Care
Power of Attorney Property / Power of Attorney Personal Care
Residential Hospice
Substitute Decision Maker
Symptoms
Terminal Illness
ICU Treatments
Arterial Line

An Arterial line (art line) is a thin plastic tube inserted into an artery to continuously measure the blood pressure. Regular blood tests are taken from it – most commonly to measure the levels of oxygen, carbon dioxide and acid within the blood.
Using local anaesthetic, the doctor inserts a needle and then the art line into the artery. The needle is removed. It is secured in place with a stitch. Although usually placed in the wrist, an art line may be positioned at the elbow, groin or foot. They commonly stay in place for several weeks. You may notice the fluid within the art line pulsating slightly. This is normal and is due to pulsations within the artery.
Balloon Pump
Bilevel Positive Airways Pressure (BIPAP)

When patients cannot breathe adequately, a BiPAP machine may provide additional oxygen and assistance with breathing. This may avoid the need to insert an ET tube (intubation). BiPAP is usually applied using a tight fitting mask to the face or nose. BiPAP is used in the ICU and sometimes in other hospital wards.
Bronchoscopy
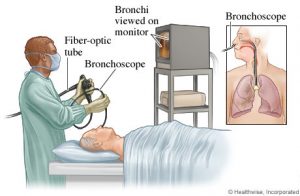 A doctor performs a bronchoscopy by passing a flexible telescope into the patient’s windpipe (trachea). This may be needed when a patient has pneumonia, when there is a blockage in the airways or to aid the placement of other tubes (e.g. a tracheostomy) into the trachea. The doctor may take samples from the airways for analysis. Occasionally a small piece of lung tissue (biopsy) is taken. In ICU bronchoscopy is usually performed through a breathing tube (ET tube or tracheostomy). Sedation is given during the procedure.
A doctor performs a bronchoscopy by passing a flexible telescope into the patient’s windpipe (trachea). This may be needed when a patient has pneumonia, when there is a blockage in the airways or to aid the placement of other tubes (e.g. a tracheostomy) into the trachea. The doctor may take samples from the airways for analysis. Occasionally a small piece of lung tissue (biopsy) is taken. In ICU bronchoscopy is usually performed through a breathing tube (ET tube or tracheostomy). Sedation is given during the procedure.Cardiopulmonary Resuscitation (CPR)

Cardiopulmonary resuscitation (CPR) is a medical procedure that attempts to restart your heart and breathing when the heart and/or lungs stop working unexpectedly. CPR can include assistance with breathing and pumping of the chest and electric shocks to try and restart the heart. If the patient survives, they will require a breathing machine and will be transferred to the ICU. CPR can be useful in some situations, but not in all situations. To learn more about CPR and whether it is right for you or your family member, see our CPR Video Decision Aid.
Central Venous Catheter (CVC), Central Line or CVP Line

A CVC is a thin plastic tube inserted into a large vein for the administration of intravenous medications and to monitor pressures within the body. Under sterile conditions a doctor inserts the CVC using a needle into either the neck, beneath the collar bone or in the groin. The needle is removed after the line has been placed. The CVC may stay in place for several weeks but will be removed as soon as it is no longer required.
Dialysis

Patient in a clinic during the dialysis.
Patients often require a dialysis machine when there is kidney failure or abnormal levels of acid and salts within the blood. It is also occasionally used to treat some drug overdoses. A doctor inserts a dialysis catheter (also known as a Vascath or Shiley) into a large vein in the neck or groin. Blood circulates through the dialysis machine, toxins are removed and the blood then returns to the body. As patients recover, the kidney function often improves and the dialysis machine can be stopped.
Extra Corporeal Membrane Oxygenation (ECMO), or EXTRA CORPOREAL LIFE SUPPORT (ECLS)

ECMO is only used in the sickest of intensive care patients when the heart and/or lungs are failing to respond to other treatments. Under sterile conditions a doctor inserts tubing into blood vessels in the neck, the groin or directly into the blood vessels near the heart (through the front of the chest in the operating theatre). Blood is drawn out of the body and into the ECMO machine where oxygen is added to it. The blood is then returned either into an artery or a vein. This keeps a patient alive while allowing time for the heart and/or lungs to recover.
Enteral Nutrition
 Enteral nutrition is a liquid form of nutrition which is passed into a patient’s stomach via a plastic tube inserted into the nose (NG tube) or mouth (OG tube). Patients who are attached to ventilators are not able to eat food the normal way. Most intensive care patients are fed in this way.
Enteral nutrition is a liquid form of nutrition which is passed into a patient’s stomach via a plastic tube inserted into the nose (NG tube) or mouth (OG tube). Patients who are attached to ventilators are not able to eat food the normal way. Most intensive care patients are fed in this way.
External Ventricular Drain (EVD)

An EVD is placed in a patient’s head to measure the pressure within the brain and to sample & drain spinal fluid (cerebro-spinal fluid or CSF). They are used in patients with severe head injury, brain haemorrhage or after neurosurgery. The EVD is inserted under strict sterile conditions by a neurosurgeon either in the ICU, emergency department or in the operating theatre.
Feeding tube

A feeding tube is a form of life support used to feed someone who can no longer swallow food. Nasogastric tubes and gastrostomy tubes are two common types of feeding tubes. Nasogastric tubes are inserted through the nose and pass down into the stomach or intestines. Orogastric tubes are inserted through the mouth and pass down into the stomach or intestines. Gastrostomy tubes are inserted through the abdomen into the stomach or intestine.
Chest Tube

Patients who have had chest or heart surgery, or trauma may need a Chest tube, a tube inserted through the chest wall to drain fluid or air from around the lung (or heart). A Chest tube may also be required to drain collections of fluid from the chest in other circumstances (such as pneumonia). Every Chest tube is inserted by a doctor under strict sterile conditions. It may be inserted while the patient is in the emergency department, operating theatre or intensive care unit. It is stitched in place underneath the armpit or at the base of the breastbone. The Chest tube is connected to a drainage bottle or collection system positioned at the side of the bed. You may see fluid in the tubing going up or down or bubbling.
Inotropes
Inotropes are drugs given to increase the blood pressure and support the function of the heart. They are given via a CVC (see CVC) into a large vein. Different types of inotrope (e.g. adrenaline, noradrenaline, milrinone) are used in various situations. Inotropes are commonly used in the ICU.
Intravenous (IV)

An intravenous (IV) is a way to give you fluids or medicine through a vein in your hand or another part of your body.
Intravenous Cannula (IVC)
Also known as IVC, or IV cannula Drip.

An intravenous cannula is a small, soft piece of hollow tubing inserted into a vein, usually in the back of the hands or the arms, which is then used to administer intravenous medications and fluids. They are used as an alternative to CVC (see CVC) when the latter is not required.
Intubation

If a patient is unconscious or has severe breathing difficulty, then an ETT is placed into the windpipe (trachea). This is then connected to a breathing machine known as a ventilator. The ventilator provides assistance with breathing and additional oxygen. A general anaesthetic is given and a doctor inserts an ETT into the trachea via the mouth (or occasionally via the nose). Sometimes the procedure is done under local anaesthetic using a flexible telescope (see Bronchoscopy). Once the ETT is confirmed to be in the right place it is secured with a special holding device. The ETT can be uncomfortable for some people; sedation may be given for comfort while the ETT is in place.
Life Support

Life support is any treatment that replaces or supports a failing bodily function without fixing the underlying problem. Life support can mean medical or surgical procedures such as a feeding tube, breathing machines, kidney dialysis or CPR. All of these use artificial means to restore and/or continue life. Without them, the patient would die.
You may have several different discussions with the health care team about life support, including whether to start life support or not, whether to continue life supports once they have been started or if there should be more or fewer life support treatments.
Lumber Puncture (LP)

An LP is performed to sample the fluid from around the spinal cord and brain. Under sterile conditions a doctor inserts a small needle through the lower part of the back and draws off a small amount of fluid. An LP may be done to measure the pressure inside the spine and brain or to check for conditions such as meningitis.
SWAN GANZ CATHETER PULMONARY ARTERY CATHETER (SWAN)
A Swan is a thin piece of tubing inserted via a vein in the neck or just beneath the collar bone. Under sterile conditions a doctor inserts the Swan using a needle. The needle is removed when the Swan is in place. The tubing then passes through the heart chambers and into the main blood vessel in the lungs (the pulmonary artery). It is used routinely during heart surgery and also when patients need large doses of medications (inotropes) to support the blood pressure and heart function. A Swan measures how well the heart is functioning and monitors pressures within the heart and lungs.
TRANS-ESOPHAGEAL ECHO (TEE)
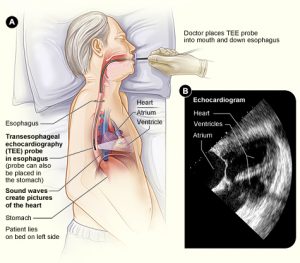 A TEE is a specialised ultrasound examination of the heart. A doctor passes an echo probe through the mouth of a patient and into the gullet (oesophagus) and then the stomach. This allows inspection of the heart and major blood vessels from inside the chest to see if there are any abnormalities. It also provides information on how well the heart is working. Sedation is given to the patient during the procedure.
A TEE is a specialised ultrasound examination of the heart. A doctor passes an echo probe through the mouth of a patient and into the gullet (oesophagus) and then the stomach. This allows inspection of the heart and major blood vessels from inside the chest to see if there are any abnormalities. It also provides information on how well the heart is working. Sedation is given to the patient during the procedure.Total PARENTERAL NUTRITION INTRAVENOUS FEEDING (TPN)
 TPN involves introducing nutrition directly into a patient’s vein. It is usually given via a CVC (see CVC). It is used when it is not possible to feed a patient via the stomach and gut. It is often possible to switch back to normal feeding via the gut as the patient’s condition improves.
TPN involves introducing nutrition directly into a patient’s vein. It is usually given via a CVC (see CVC). It is used when it is not possible to feed a patient via the stomach and gut. It is often possible to switch back to normal feeding via the gut as the patient’s condition improves.Tracheostomy

When a patient is attached to a ventilator for a prolonged period, a tracheostomy is usually performed. This is a plastic tube placed directly into the windpipe (trachea) through the front of the neck. It is more comfortable than a breathing tube through the mouth and often improves liberation from the ventilator. Under a general anaesthetic and with local anaesthetic and strict sterile precautions, a doctor performs a small operation to insert the tracheostomy. This is usually performed in the intensive care unit, although sometimes in the operating room. Speech and swallowing are sometimes possible when a patient has had a tracheostomy in for some time. The tracheostomy may ultimately be removed when the patient has recovered, leaving a small scar.
Transfusion

Blood transfusions are required to correct low blood counts (low haemoglobin, anaemia) or replace blood loss due to bleeding. Other blood products listed above are used to correct abnormal or low levels of clotting factors (if a patient is bleeding or is at risk of bleeding during a procedure) and antibodies.
Urinary Catheter

A Urinary Catheter (IDC) is a soft tube inserted into the bladder through the urethra. It drains urine from the bladder continuously, removing the need for a patient to empty the bladder on their own. A small balloon at the tip of the catheter holds it in place within the bladder. It is essential for patients who are heavily sedated, have an epidural catheter in place, or who have limited mobility and are therefore unable to walk to the toilet. It is also used to closely record urine output. The catheter is connected to a drainage bag which holds and records the amount of urine passed.
Vascath

A Vascath is a tube inserted into a large vein for dialysis (when there is kidney failure – see Dialysis) or for plasmapheresis (the removal of certain proteins from the blood). It is similar to a CVC. Under sterile conditions a doctor inserts a needle and then the vascath into either the neck, beneath the collar bone or in the groin. The needle is removed and the vascath is left in place for up to several weeks. The vascath is removed when it is no longer needed.
Ventilator

When patients cannot breathe adequately or have decreased level of consciousness, they may need to be attached to a ventilator (via an ET tube or tracheostomy – see Intubation and Tracheostomy). This is a common reason for admission to an intensive care unit. The ventilator provides additional oxygen and assistance with breathing. Patients on ventilators via an ETT often require sedation. When a patient no longer needs ventilator support it is weaned and the ETT removed. If a patient requires ventilator support for a long period of time (usually more than 10 days) a tracheostomy is commonly required.
Who’s Who in the ICU?
There are many health professionals working in the ICU, including:
Doctors
Nurses
Respiratory Therapists (RT)
Social workers
Physiotherapists (Also Known As Physical Therapist)
Pharmacists
Nutritionists and Dieticians
Spiritual Support
Unit Clerks
Volunteers
Clinical Ethicist

